The Basic Principles Of Dementia Fall Risk
The Basic Principles Of Dementia Fall Risk
Blog Article
Getting The Dementia Fall Risk To Work
Table of Contents6 Easy Facts About Dementia Fall Risk ShownThe Best Guide To Dementia Fall RiskDementia Fall Risk - TruthsA Biased View of Dementia Fall Risk
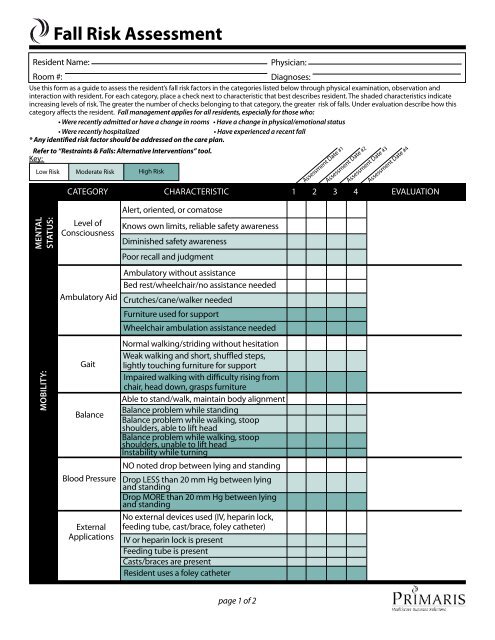
A loss threat evaluation checks to see just how likely it is that you will fall. It is primarily provided for older grownups. The assessment usually includes: This includes a collection of inquiries regarding your total health and if you've had previous drops or problems with equilibrium, standing, and/or strolling. These tools examine your stamina, balance, and gait (the means you stroll).Interventions are suggestions that might lower your danger of falling. STEADI includes three steps: you for your threat of dropping for your threat factors that can be enhanced to attempt to prevent falls (for instance, equilibrium troubles, damaged vision) to reduce your risk of dropping by utilizing effective approaches (for example, offering education and learning and resources), you may be asked numerous concerns including: Have you fallen in the previous year? Are you worried about falling?
After that you'll take a seat once again. Your company will certainly inspect the length of time it takes you to do this. If it takes you 12 secs or more, it might suggest you go to greater danger for an autumn. This test checks strength and balance. You'll being in a chair with your arms went across over your breast.
Relocate one foot midway forward, so the instep is touching the big toe of your other foot. Relocate one foot totally in front of the other, so the toes are touching the heel of your various other foot.
The Main Principles Of Dementia Fall Risk
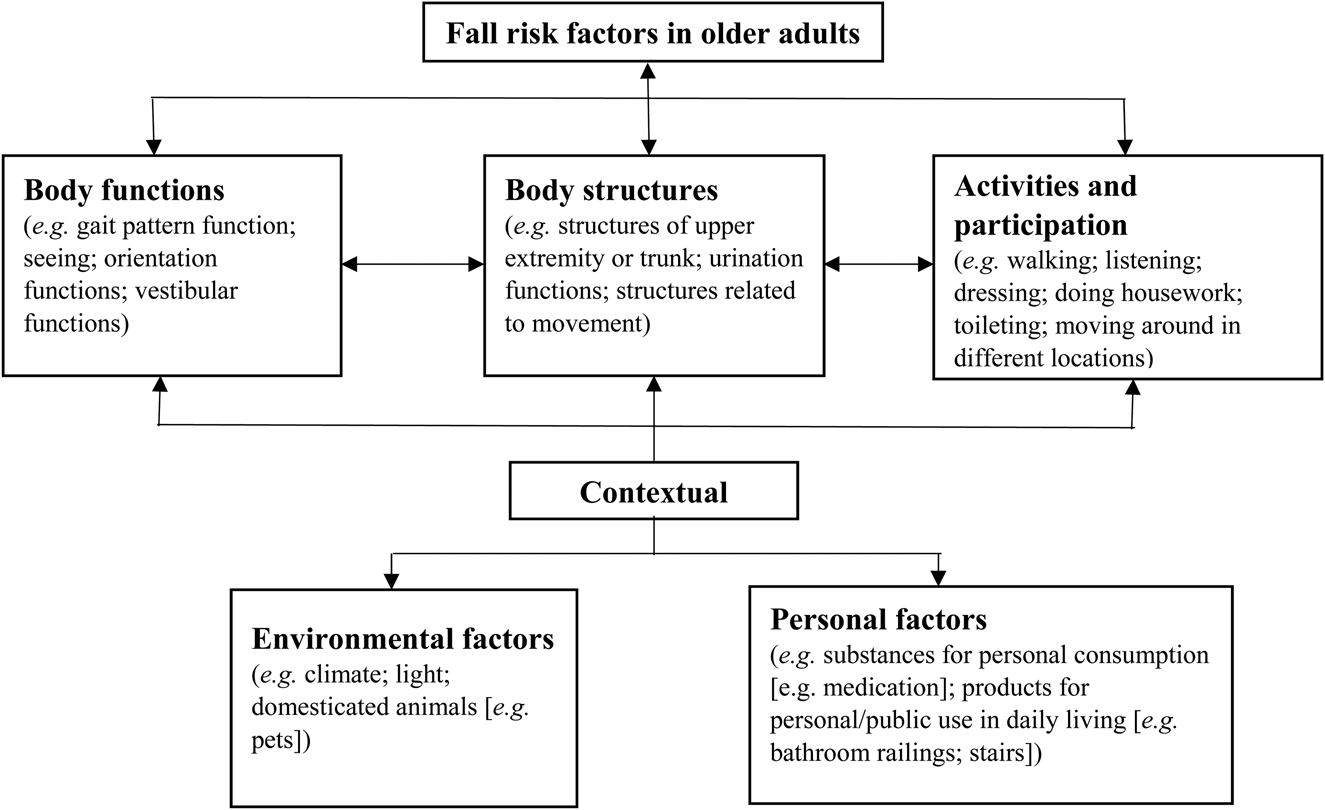
A lot of drops occur as a result of multiple contributing variables; for that reason, managing the danger of dropping starts with identifying the elements that add to drop risk - Dementia Fall Risk. A few of one of the most appropriate risk elements include: Background of prior fallsChronic medical conditionsAcute illnessImpaired gait and balance, reduced extremity weaknessCognitive impairmentChanges in visionCertain risky medicines and polypharmacyEnvironmental factors can additionally raise the threat for drops, including: Inadequate lightingUneven or damaged flooringWet or slippery floorsMissing or harmed hand rails and order barsDamaged or improperly equipped tools, such as beds, mobility devices, or walkersImproper usage of assistive devicesInadequate supervision of individuals living in the NF, consisting of those that show hostile behaviorsA effective loss risk monitoring program requires a detailed clinical evaluation, with input from all members of the interdisciplinary team
The care plan need to also include interventions that are system-based, such as those that promote a safe environment (appropriate lighting, hand rails, order bars, and so on). The performance of the treatments must be examined regularly, and the treatment plan revised as essential to mirror adjustments in the autumn danger evaluation. Applying a fall risk management system making use of evidence-based ideal method can decrease the prevalence of drops in the NF, while limiting the potential for fall-related injuries.
All About Dementia Fall Risk
The AGS/BGS standard suggests evaluating all adults matured 65 years and older for fall threat each year. This screening consists of asking individuals whether they have actually dropped 2 or more times in the previous year or sought medical focus for an autumn, or, if they have actually not fallen, whether they really feel unsteady when strolling.
Individuals that have actually fallen as soon as try here without injury must have their balance and stride examined; those with gait or equilibrium abnormalities need to get added analysis. A background of 1 fall without injury and without gait or equilibrium problems does not warrant additional analysis past continued annual autumn danger testing. Dementia Fall Risk. A fall best site danger analysis is called for as component of the Welcome to Medicare examination
The Buzz on Dementia Fall Risk
Documenting a falls history is one of the quality indicators for loss avoidance and management. A crucial component of risk analysis is a medication testimonial. A number of courses of medicines boost loss threat (Table 2). copyright medicines in particular are independent predictors of falls. These medications tend to be sedating, modify the sensorium, have a peek at these guys and impair balance and stride.
Postural hypotension can frequently be alleviated by reducing the dosage of blood pressurelowering medicines and/or stopping drugs that have orthostatic hypotension as a side effect. Use above-the-knee assistance pipe and resting with the head of the bed elevated may also reduce postural decreases in blood pressure. The suggested elements of a fall-focused physical exam are received Box 1.

A TUG time better than or equivalent to 12 seconds suggests high loss threat. Being unable to stand up from a chair of knee height without utilizing one's arms shows boosted fall risk.
Report this page